COPD- Keyword Analysis
Topics/keywords: ‘COPD’, ‘chronic obstructive pulmonary disease’
Data types: posts, comments, likes, polls
Geographical segment: global physicians, physicians by region
Analyzed data points on G-Med: 8,679
Specialties: Respiratory Medicine/Pulmonology, General Practice, Family Medicine
Countries analyzed: 59
Reach: 35,720
Introduction
This report presents a focused analysis of physician discussions on COPD (Chronic Obstructive Pulmonary Disease) using data extracted from the G-Med platform. The analysis is based on unique posts and unique comments, and have been derived through thematic keyword extraction, sentiment classification, and country-level comparison of clinical approaches. Multilingual posts were translated where necessary to ensure consistency in analysis.
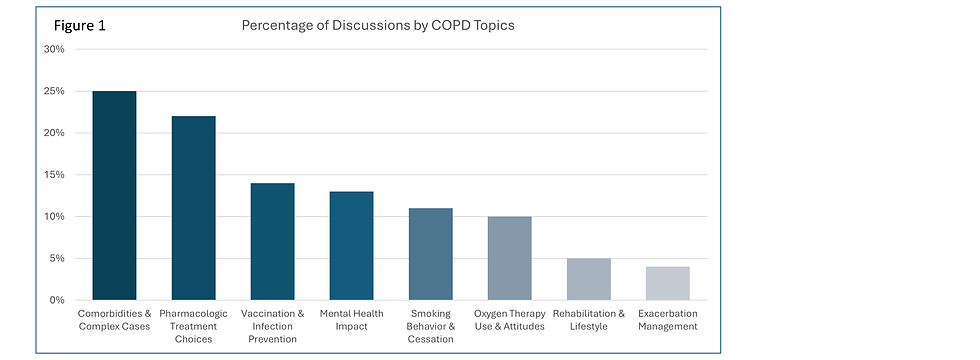
Main Concerns of G-Med Physicians on the Topic of COPD
.png)
Comorbidities and Complex Cases (25% of physician discussions)
Physicians frequently highlighted the burden of managing COPD alongside other chronic conditions such as heart failure, diabetes, anemia, and hypertension. These discussions focused on treatment complexity and prioritization, and the risk of poor outcomes due to overlapping disease pathways. There was a strong emphasis on multidisciplinary team coordination and individualized care planning.Pharmacologic Treatment Choices (22%)
A large portion of the conversation centered on the selection and adjustment of inhaled therapies, including the use of LABA/LAMA combinations, inhaled corticosteroids, and step-up or step-down regimens. Physicians debated the appropriateness of different drug classes, addressed side effects, and considered variations in patient response.Vaccination and Infection Prevention (14%)
Physicians emphasized the role of immunization, particularly against influenza, pneumococcus, and COVID-19, in preventing exacerbations and reducing hospitalization risk. Discussions included both guideline-based recommendations and physician experiences with vaccine uptake, patient resistance, and timing of administration.Mental Health Impact (13%)
Many physicians addressed the psychological burden of living with COPD, with depression, anxiety, and panic attacks emerging as frequent concerns.These issues were often linked to disease severity, social isolation, and the emotional effects of breathlessness. Some posts explored the need for integrated mental health support in COPD management.Smoking Behavior and Cessation (11%)
Physicians described a range of smoking-related challenges, from patient refusal to quit, to relapse after initial cessation efforts. Discussions also touched on cessation counseling, nicotine replacement strategies, and the psychological dynamics of long-term tobacco dependence.Oxygen Therapy Use and Attitudes (10%)
Discussions on long-term oxygen therapy (LTOT) covered technical use, indications, and patient adherence. Physicians shared experiences with both successful symptom relief and complications such as poor compliance, mobility restrictions, or psychosocial stigma related to oxygen equipment.Pulmonary Rehabilitation and Lifestyle (5%)
Although less frequent, some posts emphasized the value of non-pharmacologic interventions such as exercise training, and physiotherapy. These were often framed as adjuncts to medical therapy, particularly for improving quality of life and reducing exacerbation risk.COPD Exacerbation Management (4%)
A small subset of discussions focused on acute exacerbations, including emergency care, hospitalization criteria, and short-term use of bronchodilators or steroids. Some posts raised questions about predictors of exacerbations and optimal discharge planning.

Key Points on Diagnosis, Treatment, and Follow-Up

Diagnosis (14% of physician discussions)
Underuse of Objective Testing: Spirometry and pulmonary function tests were underutilized, with some posts expressing concern over misdiagnosis.
Overlapping Diagnoses: Physicians noted difficulties distinguishing COPD from other causes of chronic cough or dyspnea.
Delayed Recognition: Cases of advanced disease with no prior diagnosis were reported, especially in resource-limited settings.
Treatment (27%)
Inhaled Therapy as Mainstay: Bronchodilators and ICS/LABA combinations were commonly mentioned, often with mixed opinions on efficacy.
Steroid Concerns: Some discussions raised caution about chronic corticosteroid use due to systemic side effects.
Antibiotics and Acute Management: A subset of physicians discussed use of antibiotics during exacerbations, though some questioned overuse.
Follow-Up (12%)
Oxygen Dependence Management: LTOT was discussed frequently, often in the context of patient lifestyle and compliance.
Lack of Standardization: Posts revealed inconsistent follow-up protocols and rare mention of structured rehabilitation programs.
Patient Compliance Issues: Physicians cited frequent challenges with treatment adherence, especially in those with cognitive or emotional barriers.
.png)
Geographical Analysis of Physician Discussions on COPD

Of the 59 countries analyzed, the following topics were discussed in prominent countries:
United States: High engagement with inhaler regimens, adherence issues, and long-term oxygen therapy. Smoking cessation and patient education were also common themes.
France: Emphasis on pharmacologic transitions and oxygen therapy. Vaccination practices and inhaler misuse were recurring discussion points.
Germany: Focus on exacerbation response, rehabilitation, and lifestyle modification. Mental health impacts and care integration were also noted.
United Kingdom: Discussions centered on treatment escalation, smoking cessation programs, and vaccination adherence within structured care systems.
Spain: Attention to quality-of-life interventions, physiotherapy, and the cardiovascular burden in elderly patients with COPD.
Canada: Vaccination, smoking cessation, and access to care in remote areas were prominent themes. Integration of COPD management in primary care was emphasized.
Brazil: Frequent discussion of comorbidities, especially diabetes and heart failure. Concerns included patient compliance and healthcare system limitations.
Mexico: Strong focus on diagnostic delays and the burden of comorbidities. Physicians frequently cited limited access to pulmonary rehabilitation and challenges in early detection.
Australia: Physicians highlighted early intervention, multidisciplinary care, and strong support for vaccination as key components of effective management.
Argentina: Notable themes included oxygen therapy adherence, device usage, and frustration over gaps in system-level COPD care.
Cross-Country Differences in COPD Management
This section highlights dimensions where physician discussions diverged across countries.
1. Standardized vs. Personalized Follow-Up
This theme contrasts structured, protocol-driven follow-up with flexible, patient-adapted strategies.
Standardized Follow-Up: Most prominent in the United Kingdom, Canada, and Spain. These discussions emphasized routine monitoring, fixed intervals, and adherence to clinical protocols.
Personalized Follow-Up: This was rarer but visible in Australia, the United States, Germany, and Switzerland. Mentions referenced adjusting follow-up based on patient comorbidities, recovery trajectory, or psychosocial needs.
While structured care dominates, these results suggest a gradual shift toward more individualized COPD management, especially in high-income countries.
2. Confidence vs. Concern in Oxygen Therapy
This theme reflects diverging views on LTOT, ranging from clinical confidence to concern over risks.
Confidence: Strongest in the United States, United Kingdom, and Australia, where physicians reported symptom relief, quality-of-life improvements, and patient satisfaction with LTOT.
Concern: Most prominent in Germany, France, Spain, Mexico, and Brazil, with physicians citing dependence, stigma, and limited mobility. Psychological burden was a recurring subtheme in these countries.
These divided attitudes highlight regional differences in perceived value versus burden of LTOT, likely influenced by health system structures and cultural framing.
3. Smoking Cessation Encouraged vs. Resigned Attitudes
This theme captured clinical optimism vs. therapeutic resignation when dealing with smoking in COPD patients.
Encouraged: Frequently promoted in the United States, United Kingdom, Canada, and France, where physicians described cessation counseling, nicotine replacement, or structured interventions.
Resigned Attitudes: Seen most prominently in Argentina and Greece. These discussions often reflected emotional fatigue, patient refusal, or perceived futility in continued cessation attempts.
.png)
Engagement Recommendations:

As can be seen from the report, there are several knowledge gaps in COPD management, particularly around inhaler technique and adherence, comorbidity coordination, and the use of long-term oxygen therapy. A traffic-driving campaign could be beneficial in this case.
G-Med's Traffic-Driving Package could be a good fit here.



.png)